Value-Based Healthcare
““Value-based healthcare is the equitable, sustainable and transparent use of the available resources to achieve better outcomes and experiences for every person.”
”
““This platform will help us improve the quality of care we can offer patients at an individual level while at the same time focusing and tailoring services to match their needs. We aim to reduce the burden on teams and realise these benefits across all of our services, knowing the evidence supports improved outcomes as part of Value In Health Care.”
”
Value-based healthcare is the aim of organising healthcare services to provide the best possible health outcomes for patients while also optimising costs.
Traditionally healthcare providers like hospitals and general practitioners receive income based on the volume of services they provide – for example a number of operations or clinics per year or coverage of a number of the local population - regardless of the outcomes achieved. In the private sector in the UK and elsewhere, most healthcare is funded through insurance or direct self-pay where, again, activity is paid for according to what takes place irrespective of how beneficial it was to the patient. This traditional model is often called “fee for service” healthcare.
Value-based healthcare is gaining prominence in the NHS as limited resources are under ever increasing pressure because of changing population demographics, greater availability of new and expensive treatments and interventions, rising patient expectations, and an increase in patients living with complex long-term conditions.
In addition, there is known to be widespread “unwarranted variation” across the NHS in terms of the availability of resources and outcomes delivered.
There are currently several large-scale NHS programmes that utilise the principles of value-based healthcare, including:
Getting It Right First Time (GIRFT) - a national programme to improve quality of care within the NHS by reducing unwarranted variations.
NHS Right Care in England – aims to use data to identify issues then develop solutions and guidance and innovation to deliver improvements for patients, populations and systems.
‘Realistic Medicine' in Scotland - aims to improve care through sharing decision-making, personalised care, and reducing waste and harm.
'Prudent Healthcare' in Wales – aims to co-produce health and wellbeing between the public, patients and professionals, allocate resources according to needs, reduce inappropriate variation using evidence-based practices consistently and transparently.
The origins of value-based healthcare are often attributed to Harvard professors, Michael Porter and Elizabeth Teisberg, whose 2006 book ‘Redefining Healthcare' set out a new framework for competition on outcomes to improve care quality and slow the acceleration of costs in the US healthcare system.
While originally focussed on the for-profit US healthcare system many of the concepts are relevant in terms of the need to optimise outcomes within the constrained resources of the NHS despite it being a single-payer system that aims to offer universal healthcare that’s free at the point of use,
Specifically, Porter and Teisburg refer to the Outcome Measures Hierarchy, that includes the health status achieved or retaining, the time and process of recovery, and the sustainability of health, and state that for organisations to deliver value for patients and payers health outcomes, and the costs of delivering those outcomes, need to be systematically measured for all patients for the full cycle of care.
This means that as well as measuring processes of care, such as waiting times and length of stay, and complications of care, such as infection rates and mortality statistics – which the NHS traditionally does very well – we need to also measure the outcomes that matter to patients, using Patient-Reported Outcome Measures (PROMs) systematically and longitudinally for all patients.
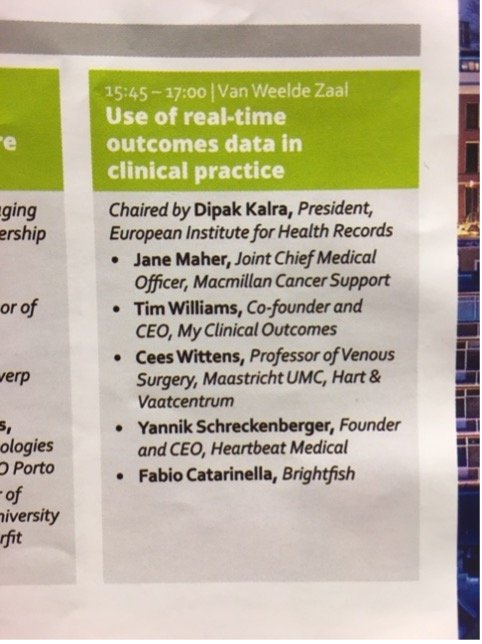
When made available in real-time outcomes data can be used:
By individuals to understand the benefits of otherwise of treatment and plan ongoing care.
At a group level to optimise and plan care services for all patients.
To identify opportunities to reduce unwarranted variation.
Ultimately to improve overall value in terms of health outcomes delivered with the resources available for the whole population.
MCO and Value-Based Healthcare
MCO CEO, Dr Tim Williams was selected for the week-long residential Harvard Business School Value-Based Healthcare Delivery Intensive Seminar in 2014. The seminar helps participants to develop a thorough understanding of value-based health care principles, including an introduction outcomes measurement and time-driven activity-based costing, through case study discussions and lectures and was taught by Prof. Porter himself as well as team of faculty and health care industry leaders.
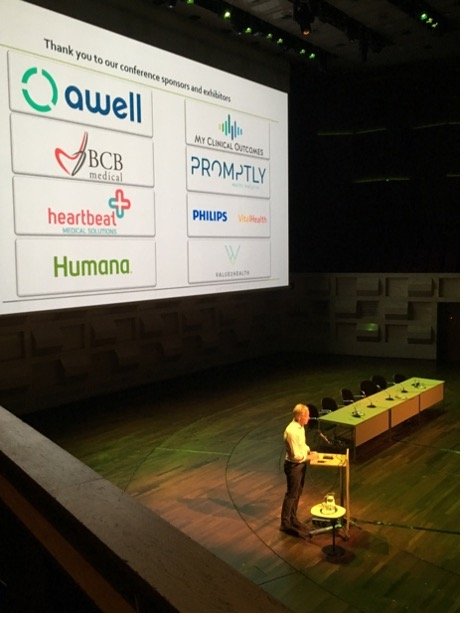
As a result of attending the seminar, My Clinical Outcomes built a relationship with the team running the newly established International Consortium of Heath Outcomes Measurement (ICHOM).
Originally founded in 2012 by Professor Porter, Dr Stefan Larsson of Boston Consulting Group, and Professor Martin Ingvar of the Karolinska Institutet in Stockholm, ICHOM aims to develop a practical framework for healthcare systems to implement the value-based healthcare framework and “to unlock the potential of value-based healthcare by defining what matters most to patients and encouraging the adoption and reporting of these measures worldwide to make life better for all”.
In 2014, My Clinical Outcomes was one of the first four technology affiliates to be recognised by ICHOM globally as being a robust and user-friendly technology platform through which providers could seek to implement the routine measurement of ICHOM Standard Sets of outcome measures.
MCO has been a regular attendee, exhibitor, and speaker at ICHOM’s international conferences, including attending the very first conference at Harvard in 2013, the second in a larger venue in Boston in 2014, London in 2016, Washington DC in 2017, Rotterdam in 2019, and virtual conferences during Covid-19. Through the affiliation the My Clinical Outcomes team has built a rich and valuable network of experts and collaborators working internationally to further the Value-based Healthcare agenda. As a result, our technology and support processes have remained up-to-date with latest developments and continues to evolve in-line with best practice and user needs from professionals working in the Value-based Healthcare arena around the world.





MCO and Cardiff & Value University Health Board – NHS Wales
NHS Wales’ commitment to value-based healthcare, underpinned by the concept of Prudent Healthcare which was first launched as a policy in January 2014.
Since the Covid-19 pandemic, health and care organisations have accelerated the development of their value-based healthcare approaches, which includes better collection and reporting of outcome data for a range of medical conditions to identify unwarranted variation in services enabled by digital transformation.
The last year has seen the creation of the PROMs standard operating model (PSOM) to allow a common approach to the capture and use of PROMs across Wales, from software to support direct care through to the development of interoperability and data standards.
In 2021 Cardiff and Value University Health Board launched a public tender to identify a a PROMs solution to partner with to develop an ambitious programme, in Welsh and English, to expand to upwards of 50 clinical areas. MCO was announced as the successful bidder and work started in early 2022.
“This programme, grounded in our approach to Value Based Healthcare, will not only help transform the collection of patient data via a digital platform; it will provide greater insight into how we can make improvements to treatments informed by what patients tell us about their physical health and wellbeing.
Putting patients at the centre of healthcare, this collaboration results in the collection and aggregation of data that supports joint decision making with patients on their care, this work will help inform how to shape services over time with a clear aim to deliver better outcomes for patients at reduced cost.”
In parallel, MCO has bid to be part of an All Wales Patient Reported Outcome Measures (PROMs) Solution Framework to provide a PROMs service to other Health Board in a standardised way whilst also supporting the Welsh Value in Health Centre’s national programme agenda.
““We are seeing the quality of care we are able to offer patients at an individual level increase while at the same time focusing and tailoring services to match their needs. The potential for reducing burden on teams and realising those benefits right across all of our services is a genuinely noteworthy prospect.”
”
““PROMs now live in NETS, Myeloma & MSK in June, then Rhinosinuitis, Mental Health using for risk strat. Over 30 specialties on our backlog already & we are only at the start of our journey!”
”
For more information about Cardiff & Vale and MCO:
Roll-out with MCO in the summary “Digital PROMS – Better patient insights, part of our approach to Value Based Healthcare” and the the Welsh Value in Health Centre’s Strategy to 2024.
Other MCO work on value-based healthcare:
EIT Health’s report on “Implementing Value-Based Healthcare in Europe: Handbook for Pioneers” features MCO work with Spire Healthcare on pages 22 and 23 and with Novartis on page 29.
MCO’s work with US health policy veteran David Introcaso on opportunities to share learning between the US and UK:
Joint essay was published in 2018.
The Healthcare Policy Podcast episode where CEO, Dr Tim Williams, discusses how/why MCO was formed, how PROMs measures are used in the clinical practice setting and more.